
異位骨化(heterotopic ossification,HO),即在關(guān)節(jié)或軟組織中出現(xiàn)病理性骨組織, 包括遺傳性HO和創(chuàng)傷性HO兩類,前者是一種進(jìn)行性骨化癥,后者常見(jiàn)于關(guān)節(jié)手術(shù)[全髖關(guān)節(jié)置換術(shù)、骨盆和肘關(guān)節(jié)手術(shù)等]術(shù)后、爆炸傷、神經(jīng)損傷和燒傷等嚴(yán)重創(chuàng)傷 [1-3]。相關(guān)研究發(fā)現(xiàn),單純肘關(guān)節(jié)脫位后HO發(fā)生率為3%[4],肘關(guān)節(jié)骨折術(shù)后HO發(fā)生率為7%[5]。HO通常會(huì)導(dǎo)致嚴(yán)重疼痛、關(guān)節(jié)僵硬、關(guān)節(jié)活動(dòng)受限等[6],嚴(yán)重影響患者的功能康復(fù)和生活質(zhì)量。由此可見(jiàn),HO已經(jīng)成為肘關(guān)節(jié)創(chuàng)傷后康復(fù)所面臨的巨大挑戰(zhàn)。
近期,我科就收治了一位肘部創(chuàng)傷術(shù)后HO伴關(guān)節(jié)活動(dòng)障礙的患者。患者戴某,男,43歲,因外傷致左橈骨小頭、尺骨冠狀突骨折行左側(cè)橈骨小頭置換術(shù)后HO伴關(guān)節(jié)活動(dòng)受限1月余門診收治入院,經(jīng)查體患者左肘屈曲、伸直、前臂旋轉(zhuǎn)均嚴(yán)重受限,伴有明顯疼痛及腫脹,日常生活及參與能力受限。
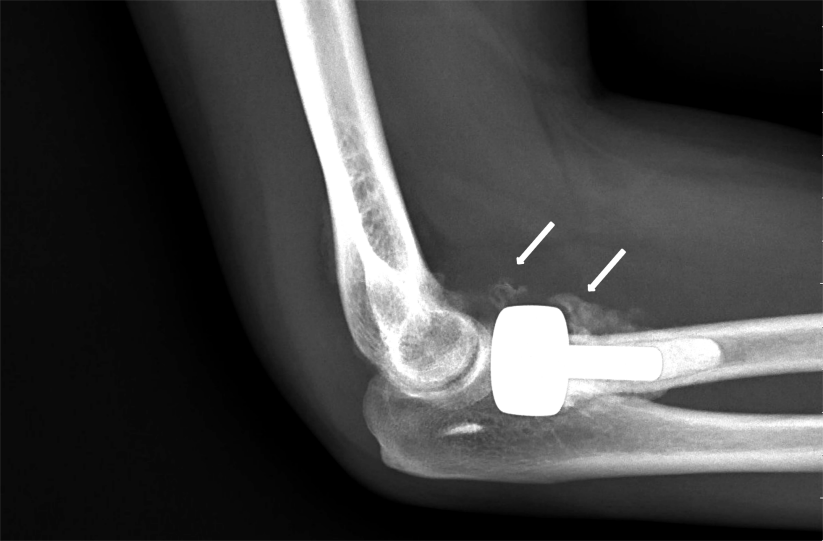
圖1:肘關(guān)節(jié)X光檢查結(jié)果
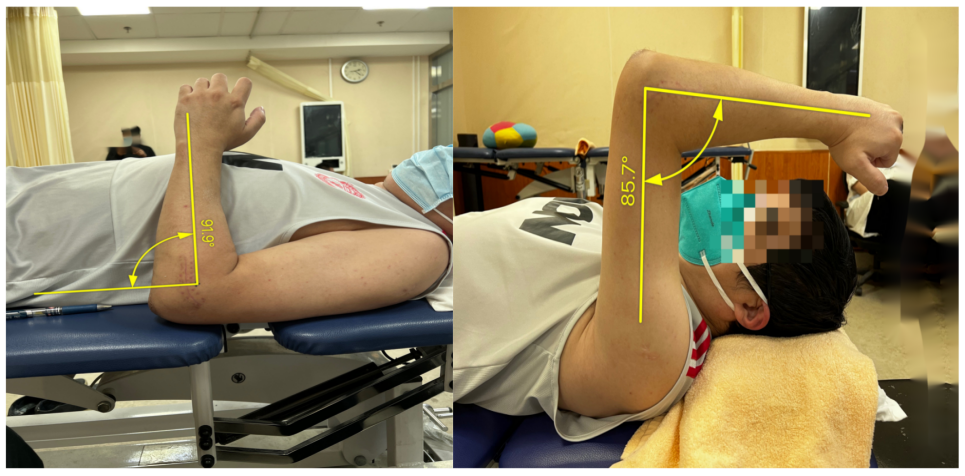
圖2:患者入院時(shí)肘關(guān)節(jié)活動(dòng)度評(píng)定
入院后,針對(duì)其HO進(jìn)展情況結(jié)合康復(fù)專科評(píng)定結(jié)果,我科康復(fù)團(tuán)隊(duì)在常規(guī)骨科術(shù)后康復(fù)治療策略的基礎(chǔ)上做了個(gè)性化調(diào)整。所有手法康復(fù)治療及家庭治療性運(yùn)動(dòng)方案設(shè)計(jì)均以低強(qiáng)度、高頻率的訓(xùn)練原則,同時(shí)考慮到創(chuàng)傷術(shù)后2月余,異位骨化仍可能處于進(jìn)展階段,所以禁用了溫?zé)岑煼ā⒊暡ā㈦姱煹瘸R?guī)物理因子治療。具體的康復(fù)治療及家庭治療性運(yùn)動(dòng)方案包括:
① 肘關(guān)節(jié)主/被動(dòng)關(guān)節(jié)活動(dòng)度訓(xùn)練,擴(kuò)大關(guān)節(jié)活動(dòng)度
② 關(guān)節(jié)松動(dòng)術(shù)擴(kuò)大關(guān)節(jié)間隙,恢復(fù)正常關(guān)節(jié)運(yùn)動(dòng)
③ 肌肉能量技術(shù),改善軟組織黏連及關(guān)節(jié)僵硬
④ 漸進(jìn)式鉸鏈?zhǔn)街怅P(guān)節(jié)支具,改善軟組織黏連及關(guān)節(jié)活動(dòng)度
⑤ 抗阻力量訓(xùn)練,改善上肢、前臂力量及神經(jīng)肌肉控制能力
⑥ 冷敷治療,緩解關(guān)節(jié)腫脹及疼痛
⑦ 日常生活能力訓(xùn)練(喝水、梳頭、潔面、穿衣等)
經(jīng)4周治療隨訪2周,患者肘關(guān)節(jié)疼痛及腫脹明顯改善、肘關(guān)節(jié)及前臂主被動(dòng)關(guān)節(jié)活動(dòng)度均明顯改善,日常生活及參與能力基本不受限。
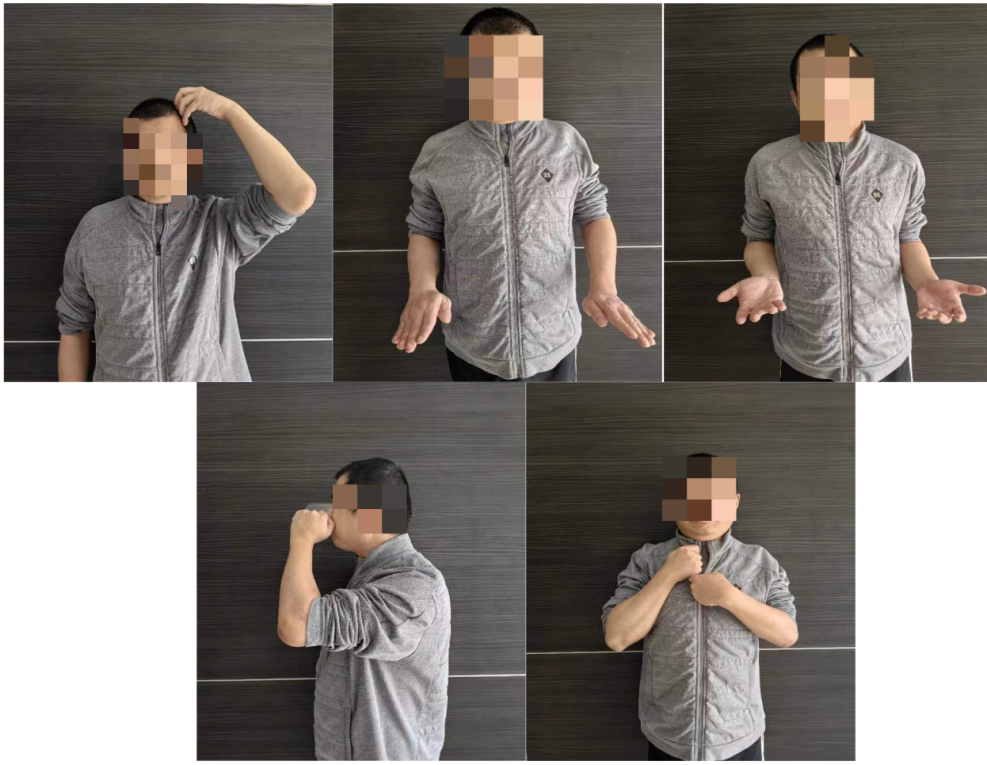
圖3:患者治療4周隨訪2周后肘關(guān)節(jié)功能活動(dòng)
總結(jié):
HO的發(fā)病機(jī)制至今仍不明確,但與之相關(guān)的風(fēng)險(xiǎn)因素通常包括創(chuàng)傷、手術(shù)、燒傷、神經(jīng)系統(tǒng)損傷等。肘部HO的發(fā)病通常發(fā)生在創(chuàng)傷、手術(shù)、燒傷或神經(jīng)系統(tǒng)損傷后兩周[7]。在HO早期階段,肘部可能表現(xiàn)為局部腫脹、紅斑、溫度升高和觸痛,很難將其與手術(shù)后的正常炎癥區(qū)別開(kāi)來(lái)[7]。
1.什么情況下應(yīng)該考慮HO呢?
HO的特征性表現(xiàn)是逐漸喪失關(guān)節(jié)活動(dòng)范圍,或者在創(chuàng)傷后炎癥應(yīng)該消退的時(shí)候肘部運(yùn)動(dòng)仍然難以恢復(fù)[8]。隨著異位骨化的進(jìn)展,疼痛、紅腫、熱可能逐漸消退,但肘部運(yùn)動(dòng)仍繼續(xù)減少。
2.哪些檢查可以幫助診斷HO?
HO的診斷主要以影像學(xué)方法(X光、CT、MRI)為主,同時(shí)需要識(shí)別先前所提到的HO高危因素,此外炎癥標(biāo)志物免疫學(xué)檢查(例如:血清堿性磷酸酶, ALP、基質(zhì)金屬蛋白酶-9,MMP-9等)對(duì)預(yù)測(cè)HO的發(fā)生也具有重要價(jià)值[9-11]。
3.針對(duì)HO如何進(jìn)行康復(fù)訓(xùn)練
對(duì)于關(guān)節(jié)創(chuàng)傷后HO的康復(fù)治療,有許多治療師和外科醫(yī)生認(rèn)為,當(dāng)懷疑或存在HO時(shí),被動(dòng)運(yùn)動(dòng)范圍(PROM)是絕對(duì)禁忌癥,因?yàn)樗赡軐?dǎo)致或加劇HO的形成[12]。但是經(jīng)過(guò)廣泛的文獻(xiàn)調(diào)研發(fā)現(xiàn),在相關(guān)研究中,會(huì)導(dǎo)致或加劇HO的運(yùn)動(dòng)被定于為“強(qiáng)制被動(dòng)運(yùn)動(dòng),F(xiàn)orcible passive movement”[12],而非專業(yè)康復(fù)治療師所實(shí)施的“被動(dòng)活動(dòng),Passive movement”[12,13]。這二者在臨床實(shí)踐中都常常被混為一談[7]。相反,早期漸進(jìn)式、持續(xù)性、低強(qiáng)度關(guān)節(jié)被動(dòng)活動(dòng)訓(xùn)練則可以有效地預(yù)防或緩解肘關(guān)節(jié)術(shù)后軟組織攣縮和關(guān)節(jié)僵硬,同時(shí)并不會(huì)對(duì)HO的發(fā)展產(chǎn)生影響[14-16]。
綜上,早期階段性、個(gè)性化的康復(fù)治療仍然是肘關(guān)節(jié)術(shù)后功能恢復(fù)的關(guān)鍵,科學(xué)合理的術(shù)后康復(fù)治療是肘關(guān)節(jié)創(chuàng)傷術(shù)后患者從容應(yīng)對(duì)HO及功能障礙的“法寶”!
參考文獻(xiàn):
1. Kassem MS, Elsayed MA Total hip replacements following acetabular fractures. 7 to 15 years clinical and radiological results. Acta Orthop Belg. 2021;87(3):419–426.
2. Kazezian Z, Yu X, Ramette M, et al Development of a rodent high-energy blast injury model for investigating conditions associated with traumatic amputations. Bone Joint Res. 2021;10(3):166–172. doi: 10.1302/2046-3758.103.BJR-2020-0367.R1.
3. Shaath MK, Lim PK, Andrews R, et al Clinical results of acetabular fracture fixation using a focal Kocher-Langenbeck approach without a specialty traction table. J Orthop Trauma. 2020;34(6):316–320. doi: 10.1097/BOT.0000000000001723.
4. Sagi HC, Jordan CJ, Barei DP, et al Indomethacin prophylaxis for heterotopic ossification after acetabular fracture surgery increases the risk for nonunion of the posterior wall. J Orthop Trauma. 2014;28(7):377–383. doi: 10.1097/BOT.0000000000000049.
5. Cheung EV, Sarkissian EJ Complications of elbow trauma. Hand Clin. 2015;31(4):683–691. doi: 10.1016/j.hcl.2015.06.012.
6. Beckmann JT, Wylie JD, Kapron AL, et al The effect of NSAID prophylaxis and operative variables on heterotopic ossification after hip arthroscopy. Am J Sports Med. 2014;42(6):1359–1364. doi: 10.1177/0363546514526361.
7. Freed JH, Hahn H, Menter R, et al The use of the three-phase bone scan in the early diagnosis of heterotopic ossification (HO) and in the evaluation of Didronel therapy. Paraplegia. 1982;20(4):208–216.
8.Hastings H, Graham TJ. The classification and treatment of heterotopic ossification about the elbow and forearm. Hand Clin. 1994;10:417–37.
9.Thomas BJ, Amstutz HC. Results of the administration of diphosphonate for the prevention of heterotopic ossification after total hip arthroplasty. J Bone Joint Surg Am. 1985;67A: 400–3.
10. Cassar-Pullicino VN, McClelland M, Badwan DA, et al Sonographic diagnosis of heterotopic bone formation in spinal injury patients. Paraplegia. 1993;31(1):40–50.
11. Garland DE A clinical perspective on common forms of acquired heterotopic ossification. Clin Orthop Relat Res. 1991;(263):13–29.
12.Casavant AM, Hastings H 2nd. Heterotopic ossification about the elbow: a therapist's guide to evaluation and management. J Hand Ther. 2006;19(2):255-266. doi:10.1197/j.jht.2006.02.009
13.Michelsson JE, Rauschning W. Pathogenesis of experimental heterotopic bone formation following temporary forcible exercising of immobilized limbs. Clin Orthop. 1983;176: 265–72.
14.Evans EB. Heterotopic bone formation in thermal burns. Clin Orthop. 1991;263:94–101.
15.Crawford CM, Varghese G, Mani M, Neff JR. Heterotopic ossi- fication: are range-of-motion exercises contraindicated? J Burn Care Rehabil. 1986;7:323–7.
16.Peterson SL, Mani MM, Crawford CM, Neff JR, Hiebert JM. Postburn heterotopic ossification: insights for management decision making. J Trauma. 1989;29:365–9.

北京清華長(zhǎng)庚醫(yī)院APP
快速掛號(hào)